Top Things to Know: Call to Action for Cardiovascular Disease in Women: Epidemiology, Awareness, Access, and Delivery of Equitable Health Care
Published: May 09, 2022
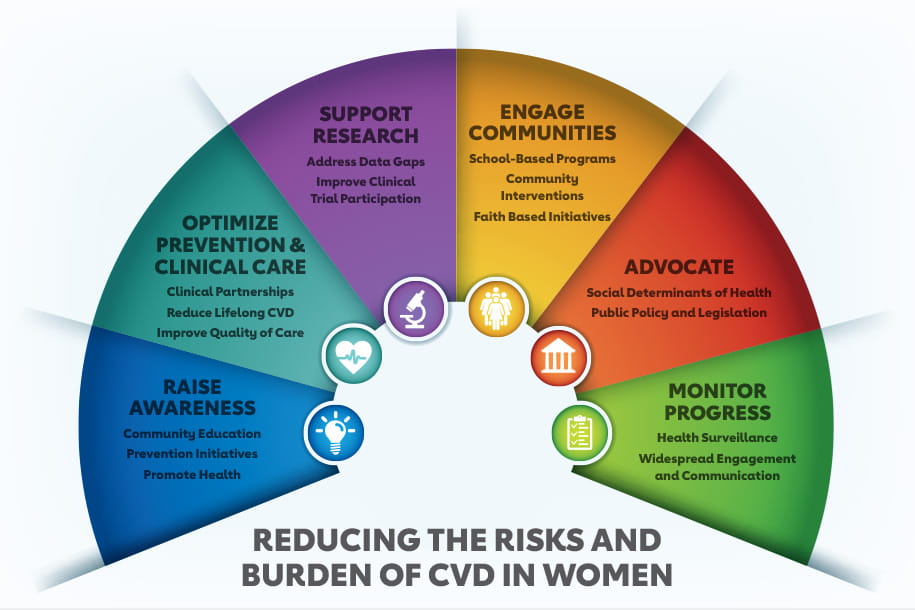
- Addressing the pervasive gaps in knowledge and care delivery to reduce sex-based disparities and achieve equity is fundamental to the American Heart Association’s commitment to advancing cardiovascular health for all by 2024.
- Cardiovascular disease remains the most common cause of death among US women and men today as was true thirty years ago.
- Nearly half (44.4%) of US females ages 20 years and older have some form of clinical CVD including hypertension.
- Women surveyed in 2019 compared to 2009 were 74% less likely to identify heart disease as their leading cause of death. with differences most apparent among younger women and those women who self-report as Hispanic or non-Hispanic Black.
- To directly address the needs of women, the AHA launched Research Goes Red in collaboration with Verily’s Project Baseline. Research Goes Red is an online platform that positions women at the center of clinical research to accelerate scientific discovery by fostering active engagement.
- Hypertension is highest in Non-Hispanic (NH) Black females, LDL cholesterol is the highest in NH White females, diabetes mellitus is highest among Hispanic females and overweight and obesity are highest in NH Black and Hispanic females. Of note, this Hispanic cohort is composed mainly of Mexican American females.
- Adverse social determinants of health (SDOH) adversely affect the prevalence and progression of CVD across all age, sex, race, and ethnicity groups. The lived experience and the magnitude of the impact of SDOH on CVD differs across such groups.
- The cardiovascular health of pregestational women in the US has declined and that of pregnant women is suboptimal, and lower than among age-matched non-pregnant women. Decreased cardiovascular health in pregestational and pregnant women increases the risk for adverse pregnancy outcomes, CVD in these women and worse cardiovascular health in their children.
- Females are disproportionately affected by systemic inflammatory and autoimmune disorders, including systemic lupus erythematosus, rheumatoid arthritis, and scleroderma. Further, when present, these risk factors greatly augment the risk of CVD events.
- The introduction of the Patient Protection and Affordable Care Act (ACA) improved access to affordable health insurance coverage for many females aged 19 to 64 years, the largest coverage gain of any group.
Citation
Wenger NK, Lloyd-Jones DM, Elkind MSV, Fonarow GC, Warner JJ, Alger HM, Cheng S, Kinzy C, Hall JL, Roger VL; on behalf of the American Heart Association. Call to action for cardiovascular disease in women: epidemiology, awareness, access, and delivery of equitable health care: a presidential advisory from the American Heart Association [published online ahead of print May 9, 2022]. Circulation. doi: 10.1161/CIR.0000000000001071