Recurrent Pericarditis for Professionals
Recurrent Pericarditis
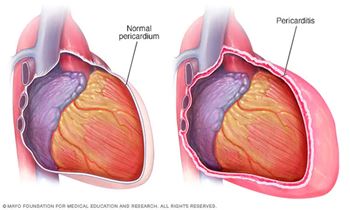
Recurrent pericarditis is a common complication after an initial episode of acute pericarditis, characterized by the recurrence of chest pain and signs of cardiovascular inflammation. Recurrent pericarditis presents major short-term and long-term challenges for clinicians and patients alike.
The impact of recurrent pericarditis often extends beyond cardiac effects, with general uncertainty of each recurrence triggering anxiety, depression, and disruption in overall quality of life.
OnDemand Videos

Recurrent Pericarditis: Practical and Surgical Management
This expert-led video covers recurrent pericarditis management, emphasizing IL-1’s role in inflammation and recurrence, treatment strategies—including cardiac surgery—and a patient’s journey.
Acute Pericarditis: A Practical Approach to Diagnostic Evaluation & Initial Management
Enhance your understanding and skills in diagnosing and managing acute pericarditis with our on-demand video, available for healthcare professionals.
Special Topics in Recurrent Pericarditis: Recognize and Manage Refractory Disease
This webinar will explore the features of monogenic autoinflammatory diseases as a paradigm for IL-1 mediated recurrent pericarditis.
Acute Pericarditis: Recognition, Initial Management, and Preventing Recurrence
This webinar reviews pericarditis diagnosis, risk stratification, treatment strategies, and practical pharmacology for management and recurrence prevention.
Recurrent Pericarditis: Epidemiology, Presentation, Pathophysiology, and Diagnostic Testing
This webinar provides key takeaways for initial diagnosis and clinical evaluation strategies in recurrent pericarditis.HeartBEATS from Lifelong Learning™
Navigating Recurrent Pericarditis: Shared Decision Making and Patient Stories
Conventional Approaches to Managing Recurrent Pericarditis
IL-1 Blockade – Rationale, Evidence Base, and Practical Clinical Pharmacology
This vodcast helps healthcare professionals understand current guidelines, science, and best practices for managing recurrent pericarditis, focusing on IL-1 blockade, supporting evidence, and clinical pharmacology to improve patient outcomes.
Clinical Evaluation and Diagnostic Assessment
In this episode, experts explore the diagnosis of acute pericarditis, highlighting key factors that influence patient care and support effective management.
Management and Pharmacological Strategies
In this episode, experts discuss the initial pharmacologic management of acute pericarditis, offering practical insights to enhance your clinical skills.
Podcasts
Long Term Complications of Recurrent Pericarditis
Presenters: Janet Kloos, RN, PhD, APRN-CCNS, CCRN; Allen Luis, MD; C. Barton Gillombardo, MD; Brian Hoit, MD
Identifying an underlying cause of the clinical features during history-taking may be beneficial. In developed nations, idiopathic and post cardiac surgery are most frequent causes of constrictive pericarditis. In developing and underdeveloped nations and in immunosuppressed patients, tuberculosis is the major cause. This podcast will review the initial diagnosis, clinical evaluation and treatment of the long-term complications of recurrent pericarditis. Listen Now!
Recurrent Pericarditis in Systemic Autoinflammatory and Autoimmune Disease – Clinical Recognition and Management
Presenters: Tevfik Ismail, MB, BS, PhD, FRCP, FACC, FAHA; Claire Peet, MD; Shreyasee Amin, MD, CM, MPH
In this podcast, experts explore in more detail the diagnosis and clinical features of monogenic autoinflammatory diseases many of which can present with recurrent pericarditis. In addition, discussion will include the spectrum of autoimmune diseases complicated by pericarditis, how to recognize these clinically, and when to call for help. Listen Now!
Recurrent Pericarditis: The Role of IL-1 Blockade
Presenters: Allen Luis, MD; Anene Ukaigwe, MD; Cyrille K. Cornelio, Pharm.D., BCCP
In 2021, the FDA-approved Rilonacept to treat recurrent pericarditis and reduce the risk of recurrence. In this podcast learn more about the role interleukin-1 (IL-1) plays in the pathophysiology of pericarditis. Listen Now!
Pathophysiology of Recurrent Pericarditis
Presenters: Paul Cremer, MD; Aisha Siraj, MD, FACC; Antonio Abbate, MD, PhD
Listen to this podcast to better understand the triggers causing recurrent episodes of pericarditis. Experts discuss how to assess those triggers to direct optimal therapy.
Beyond Acute – Recurrent Pericarditis
Presenters: Katherine E. Di Palo, PharmD, FAHA, FHFSA, BCACP, BCGP; Farshad Forouzandeh, MD, PhD, FACC, FSCAI; David Lin, MD
In this podcast, Drs. Forouzandeh, Lin, and Di Palo discuss initial management of recurrent pericarditis. Learn how to distinguish acute pericarditis from recurrent pericarditis. They will also explore diagnostic criteria and initial pharmacotherapy for recurrent pericarditis. Listen now to get more insight on care delivery strategies to improve patient outcomes and decrease associated health care costs due to recurrent pericarditis.
Treatment of Acute Pericarditis
Presenters: Tevfik F Ismail, MB, BS, PhD, FRCP, FACC, FAHA; Antonio Brucato, MD; Robert Barcelona, Pharm.D., BCPS
In this podcast, Drs. Tevfik Ismail, Antonio Brucato, and Robert Barcelona will focus on the treatment of acute pericarditis and review the relevant clinical pharmacology of the agents used. Learn more on the use of drugs that are off-label for acute pericarditis in the United States and other jurisdictions and some practical tips and tricks and pointers towards pitfalls to avoid when managing this condition.
Complications of Acute Pericarditis
Presenters: Christine L. Jellis, MD PhD FACC FASE; Tim Simpson, MD, Pharm D, and Sadeer Al-Kindi, MD, FACC.
Learn more in this podcast on the causes, complications and treatments of acute pericarditis and explore how to prevent an initial episode of acute pericarditis from evolving into recurrent pericarditis.
What is Acute Pericarditis: Signs and Signals
Presenters: S. Allen Luis, MD, PhD, FRACP, FACC, FASE; James Lloyd, MD; Janet A. Kloos, RN, PhD, APRN-CCNS, CCRN
Pericarditis is inflammation of the fibroelastic pericardial sac. Acute pericarditis has been observed in ≈0.1% of hospitalized patients and 5% of patients admitted to the emergency department with a diagnosis of noncardiac chest pain. In this podcast, learn the clinical features of Acute Pericarditis.
Addressing Recurrent Pericarditis
Guidelines and Articles
- 2014 AHA/ACC Guideline for the Management of Patients With Non-ST-Elevation Acute Coronary Syndromes (PDF)
- Cardiovascular Disease and Breast Cancer: Where These Entities Intersect: A Scientific Statement From the American Heart Association. Circulation. 2018;137:e30–e66.
- ACC/AHA/ESC 2006 Guidelines for the Management of Patients with Atrial Fibrillation - Full Text. Circulation. 2006;114:e257–e354.
Resources For Patients
