Omega-6 Fatty Acids in the Hierarchy of Cardiovascular Protection
Last Updated: March 05, 2021
As societies advance in terms of education, technology, and wealth, there is escalating interest in lifestyle interventions (e.g. nutritional strategies, physical activity, weight management) that promote cardiovascular health. This concept must be framed in the realization that atherosclerosis is anatomically present in nearly all middle-aged and older adults. Eggen and colleagues reported autopsy results in 1,242 adults and found over 50% of all individuals over age 40, and over 75% of those over age 60, had atherosclerosis in the left anterior descending coronary artery, irrespective of the cause of death.[1] Tuzcu and colleagues found the prevalence of coronary atherosclerosis varied from 17% in individuals less than 20 years old, to 85% in subjects age 50 and above, who underwent intravascular ultrasound after noncardiac death prior to heart donation for transplantation.[2] In contrast, atherosclerosis is uncommon in free-living nonhuman primates and can be induced by proatherogenic diets.[3] Thus, over the course of several decades of human life, a strong relationship between diet, the deposition of apo-B containing lipoproteins in the arterial wall, and the development of atherosclerosis is suspected.[4]
In the Scientific Advisory from the American Heart Association, led by Harris and colleagues, titled Omega-6 Fatty Acids and Risk for Cardiovascular Disease, the issue of omega-6 polyunsaturated fatty acids (PUFA) is reviewed in detail. The common forms of omega-3 and omega-6 PUFA have similar chemical structures, as shown in Figure 1. Despite theoretical concerns regarding omega-6 PUFA and inflammation and oxidative stress, there are no compelling epidemiologic or clinical trial data to suggest that omega-6 PUFA are proatherogenic. The cardioprotection debate lies in how much omega-6 PUFA should be consumed in relation to omega-3 PUFA. Expert opinion has ranged widely (1:1-1:20) for optimal omega-3 to omega-6 PUFA relative consumption in the diet.[5] Although ecologic studies suggest that a ratio of to 1:1 is compatible with human evolutionary roots, ratios of 1:16 or more are reflective of a Western diet.[6]
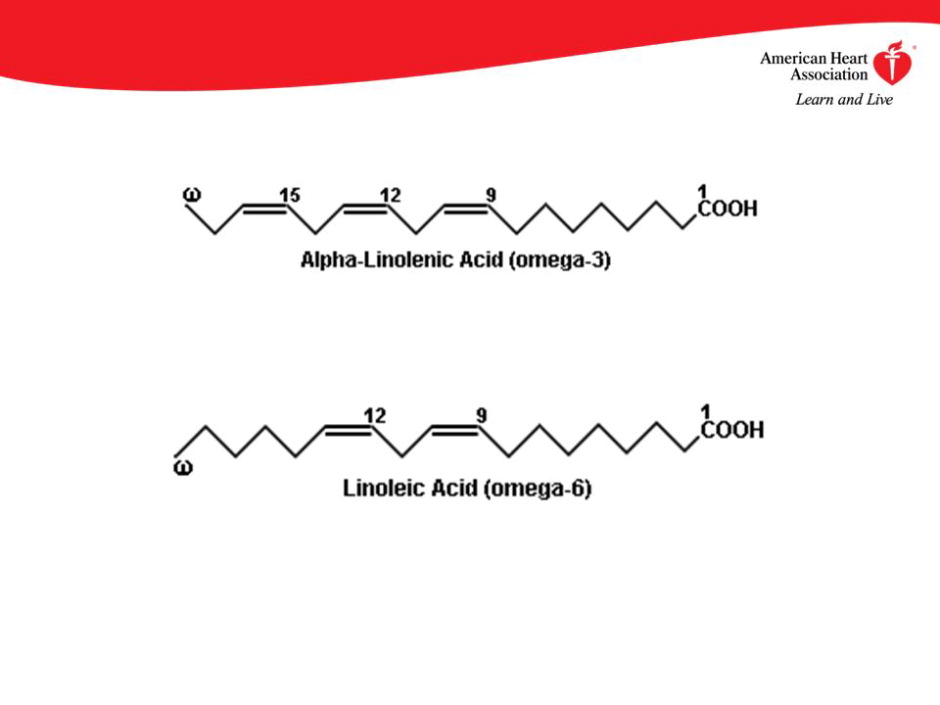
Figure 1. Chemical structures of omega-3 (alpha linolenic acid) and omega-6 (linoleic) PUFA.
Linoleic acid is an 18-carbon long PUFA that serves as the most abundant omega-6 PUFA in the human diet. As linoleic acid is absorbed and metabolized, it is converted into a derivative fatty acid, gamma linoleic acid, which is converted into di-homo-gamma linoleic acid (DGLA) and arachidonic acid (AA). These products are then converted into two types of prostaglandins (PG) by adding two carbon molecules and removing hydrogen molecules with DGLA being converted to PGE1, and AA is converted into PGE2. PGE3 is synthesized by the conversion of omega-3 PUFA. Both PGE1 and PGE3 are antiinflammatory agents and reduce platelet aggregability. PGE2, however, is inflammatory and increases platelet adhesion. All three forms must be present to achieve a rheostasis. In addition, PGE1 promotes natriuresis and diuresis, while PGE2 opposes these actions. Thus, these three types of prostaglandins, which are principal derivatives of omega-6 PUFA, serve as modulators in several homeostatic systems that relate to heart and kidney disease. When compared with saturated fatty acids, omega-6 PUFA confer a lower risk of cardiovascular events.
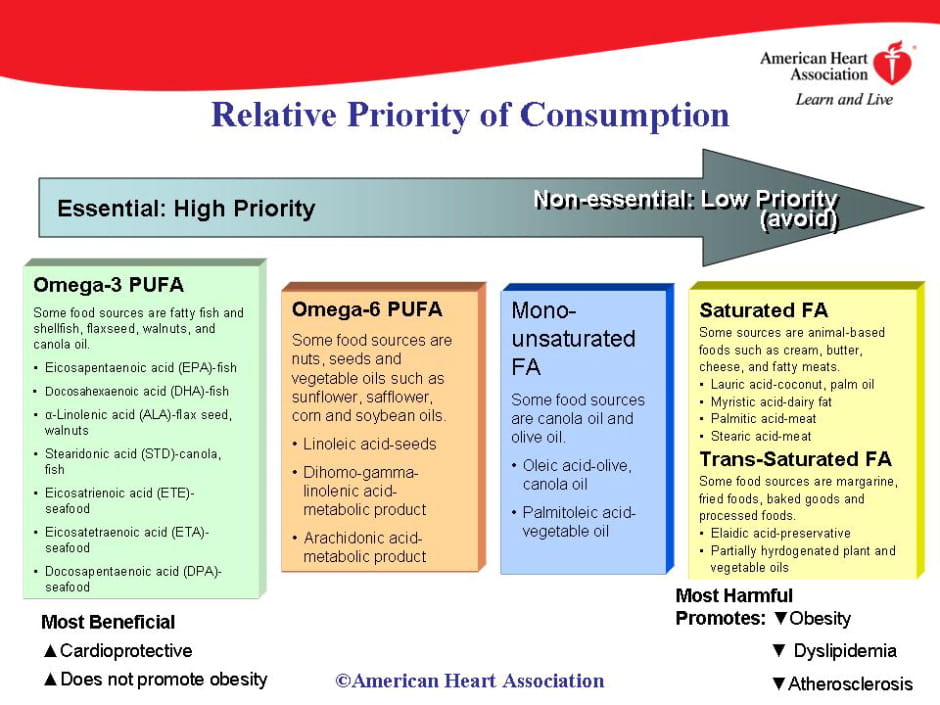
Figure 2. Continuum of fatty acids in terms of health benefits and risks.
In summary, the American Heart Association Science Advisory on Omega-6 Fatty Acids sets the record straight with respect to cardioprotective benefits and recommends intakes as a percent of energy with specific references to relevant observational studies, randomized controlled trials, and pooled data (meta-analyses). By viewing fats as a macronutrient class, omega-6 PUFA occupy a favorable position on a continuum of fat intake in a diet formulated to prevent atherosclerosis and its consequences.
Citation
Harris WS, Mozaffarian D, Rimm E, et al. Omega-6 fatty acids and risk for cardiovascular disease: a science advisory from the American Heart Association Nutrition Subcommittee of the Council on Nutrition, Physical Activity, and Metabolism; Council on Cardiovascular and Stroke Nursing; and Council on Epidemiology and Prevention. Circulation 2009. Published online before print January 26, 2009, 10.1161/CIRCULATIONAHA.108.191627.
References
- Eggen DA, Strong JP, McGill HC Jr. Coronary calcification. Relationship to clinically significant coronary lesions and race, sex, and topographic distribution. Circulation 1965;32(6):948-955.
- Tuzcu EM, Kapadia SR, Tutar E, et al. High prevalence of coronary atherosclerosis in asymptomatic teenagers and young adults: evidence from intravascular ultrasound. Circulation 2001;103(22):2705-2710.
- Strong JP, Eggen DA, Newman WP 3rd, Martinez RD. Naturally occurring and experimental atherosclerosis in primates. Ann N Y Acad Sci 1968;149(2):882-894.
- McGill HC Jr, McMahan CA, Herderick EE, et al. Origin of atherosclerosis in childhood and adolescence. Am J Clin Nutr 2000;72(5 Suppl):1307S-1315S.
- Harris WS. The omega-6/omega-3 ratio and cardiovascular disease risk: uses and abuses. Curr Atheroscler Rep 2006;8(6):453-459.
- Simopoulos AP. The importance of the omega-6/omega-3 fatty acid ratio in cardiovascular disease and other chronic diseases. Exp Biol Med (Maywood). 2008;233(6):674-688.
Science News Commentaries
-- The opinions expressed in this commentary are not necessarily those of the editors or of the American Heart Association --
Pub Date: Monday, Jan 26, 2009
Author: Peter A. McCullough, MD, MPH
Affiliation: