It’s Complicated: Challenges Inherent in Developing and Testing Complex Interventions such as Patient Centered Models of Care
Last Updated: November 26, 2024
Rossi and colleagues describe the characteristics of existing care delivery models and review the evidence of effectiveness after conducting an ambitious scoping review of models of care delivery for selected CVD conditions. Models were included in their review if they included the use of evidence-based guidelines, clinical decision support tools, and systematic evaluation processes. Importantly, the included models had to be patient-centered or include the patient's perspective in the plan of care. The review has several notable observations. The studies often failed to describe well the inter-disciplinary interactions so that they could be replicated. Also, while some studies showed process improvements, they generally failed to show improved outcomes, perhaps because of the study designs and power, but possibly also because of the interventions themselves. Moreover, the used of established definitions and outcomes varied across the studies.
The Rossi et al review expands on an earlier AHA Scientific Statement describing a taxonomy for disease management published in 2006.1 That taxonomy of 8 domains (e.g., patient population, intervention content, method of communication, environment) was intended to describe critical attributes of disease management programs to facilitate future comparisons. A lot has happened since 2006. Although the need for patient-centered care has been addressed in the CVD literature since 1958,2 a PubMed search suggests that the CVD community did not embrace patient-centered care enthusiastically until approximately 2010 when Congress authorized PCORI, the Patient Centered Outcomes Research Institute, focused on ensuring that patients and stakeholders have a seat at the research table. Prior to that, in the 2006 taxonomy we talked about "disease management" – a decidedly clinician-focused approach to the care of people with CVD. We were concerned about how best to focus our interventions to achieve our outcomes. We mentioned "patient centered" in terms of measurement (e.g., quality of life, self-management, and caregiver burden) but a true emphasis on patient-centeredness was not addressed.
Several authors have written about how best to define patient-centered.3,4 Lorig5 argues that care that is patient-centered considers the things that patients want. These elements, she argues, are 1) comprehensive care, 2) coordination of care, 3) timeliness, 4) functioning e-health or patient access to records and the opportunity to add to the record, 5) clear and reliable communication, 6) convenience, 7) respect, 8) empathy and understanding, 9) time, 10) continuity and stability, and 11) fairness. These descriptions of patient-centered are elegant but integrating these elements into models of care and testing their effectiveness is challenging and studies to date have rarely been successful in doing so. This may be because patient-centered models of care are inherently complex interventions requiring different methods of development and testing than the traditional randomized controlled trial (RCT).
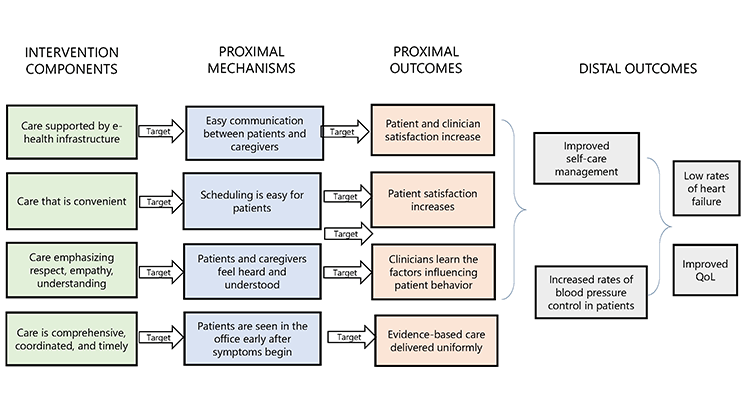
Complex interventions are those that contain several interacting components, a range of targeted behaviors, and the expertise and skills required by those delivering the intervention, among other things.6 If the individual elements of a complex intervention are themselves complex interventions, optimization research is needed before combining the individual elements for efficacy testing in a RCT.7 Collins,8 who developed the Multiphase Optimization Strategy (MOST) for optimizing elements of a complex intervention, advises that the process begins with the development of a conceptual model specifying the intervention components, proximal mechanisms, proximal outcomes, and distal outcomes targeted in the intervention. This process of theoretical deconstruction into component parts allows refinement of each part to assure that nothing unnecessary or ineffective is included.6
The list of elements proposed by Lorig5 as core to patient centered care illustrates how complicated it is to develop and test interventions that are truly patient-centered. A model of care that is comprehensive, coordinated, and timely with the support of a fully functional e-health infrastructure may look very different than one designed to provide timely responses to patient needs for clear communication, respect, empathy, understanding, convenience, and fairness. For example, an intervention addressing comprehensive care may look like the current guideline-driven model of care, with a proximal mechanism of increasing the use of evidence-based therapies. The proximal outcome might be control of blood pressure in a hypertensive population with a decrease in the incidence of heart failure as the distal outcome (Figure 1). But the intervention module addressing convenience might entail an entirely new organization of the clinic, with a proximal mechanism of increasing the ease with which patients can schedule visits. The proximal outcome might be patient satisfaction with an increase in blood pressure control of hypertensive patients as the distal outcome.
In addition to these issues, a central challenge for beneficial complex interventions is to determine their essential features and develop an implementation plan that is scalable in ways that retain their effectiveness. A further challenge is that these interventions often need customization within sites and regions, to leverage their challenges, strengths, and resources. We need more attention on the implementation science issues if we are to enable these patient-centered models to achieve their promise. Currently, we have a situation where interventions are often bespoke, dependent on individuals, and hard to replicate and scale in ways that would give us confidence about their ability to produce better outcomes. Perhaps In a digital world, platforms can be configured to have a structure that disseminates and standardizes their active ingredients while providing adaptability to match local resources and strengths. All these efforts should ensure that we are integrating the patients' preferences and goals, given that Rossi and colleagues emphasize the important point that an overlooked characteristic of the models reviewed was the lack of systematic approaches to engage patients and incorporate their unique perspectives into the treatment plan.
The review suggests that there is a great opportunity for people in the field to generate needed evidence about these patient-centered models of care. Also, there need for built-in, rapid-cycle evaluations to permit continual local iteration and accountability. We need to know what works, and how best to configure these models so they are built to scale and adaptable. Moreover, we should be developing a consortium of institutions ready to implement and test these models. In the end, we still have much work to do to enable patient-centered models to become the standards of care.
Citation
Rossi LP, Granger BB, Bruckel JT, Crabbe DL, Graven LJ, Newlin KS, Streur MM, Vadiveloo MK, Walton-Moss BJ, Warden BA, Volgman AS, Lydston M; on behalf of the American Heart Association Complex Patient and Family Care Committee of the Council on Cardiovascular Stroke Nursing; Council on Clinical Cardiology; and Council on Quality of Care and Outcomes Research. Person centered models for cardiovascular care: a review of theevidence: a scientific statement from the American Heart Association [published online ahead of print July10, 2023]. Circulation. doi: 10.1161/CIR.0000000000001141
References
- Krumholz HM, Currie PM, Riegel B, et al. A taxonomy for disease management: a scientific statement from the American Heart Association Disease Management Taxonomy Writing Group. Circulation. 2006;114(13):1432-1445.
- Wooden HE. Patient-centered cardiac care. Hospital progress. 1958;39(12):80-82 passim.
- Hearn J, Dewji M, Stocker C, Simons G. Patient-centered medical education: A proposed definition. Med Teach. 2019;41(8):934-938.
- Robinson JH, Callister LC, Berry JA, Dearing KA. Patient-centered care and adherence: definitions and applications to improve outcomes. J Am Acad Nurse Pract. 2008;20(12):600-607.
- Lorig K. Patient-Centered Care: Depends on the Point of View. Health Educ Behav. 2012;39(5):523-525.
- Skivington K, Matthews L, Simpson SA, et al. A new framework for developing and evaluating complex interventions: update of Medical Research Council guidance. BMJ. 2021;374:n2061.
- Czajkowski SM, Powell LH, Adler N, et al. From ideas to efficacy: The ORBIT model for developing behavioral treatments for chronic diseases. Health Psychol. 2015;34(10):971-982.
- Collins LM. Optimization of Behavioral, Biobehavioral, and Biomedical Interventions: The Multiphase Optimization Strategy (MOST). Pittsburgh, PA: Springer; 2018.
Science News Commentaries
-- The opinions expressed in this commentary are not necessarily those of the editors or of the American Heart Association --
Pub Date: Monday, Jul 10, 2023
Author: Barbara Riegel, PhD, RN, FAHA, FAAN; Harlan M. Krumholz, MD, SM; Harold H. Hines, Jr. Professor of Medicine
Affiliation: Professor, University of Pennsylvania School of Nursing Senior Research Scientist, Center for Home Care Policy & Research at VNS Health[;