Tachycardia: Fast Heart Rate

ECG strip showing a normal heartbeat

ECG strip showing tachycardia
Tachycardia in adults refers to a heart rate of more than 100 beats per minute. How that’s defined may depend on your age and physical condition.
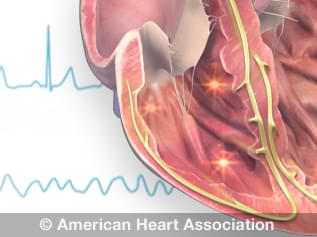
View an animation of tachycardia.
Types of tachycardias
Atrial or Supraventricular Tachycardia (SVT)
Atrial or supraventricular tachycardia (SVT) is a fast heart rate that starts in the upper chambers of the heart. Some forms of this tachycardia are paroxysmal atrial tachycardia (PAT) and paroxysmal supraventricular tachycardia (PSVT).
With atrial or supraventricular tachycardia, electrical signals in the heart’s upper chambers occur abnormally. There may also be structural abnormalities of the heart. This interferes with electrical impulses coming from the sinus node, the heart’s natural pacemaker.
The disruption results in a faster than normal heart rate. This rapid heartbeat keeps the heart’s chambers from filling completely between contractions, which may compromise blood flow to the rest of the body.
Risk factors for Atrial or SVT
In general, those most likely to have atrial or supraventricular tachycardia are:
- Children (SVT is the most common type of arrhythmia in kids)
- Women, to a greater degree than men
- Young people with anxiety
- People who are middle-aged and older
You are at increased risk for atrial tachycardia or SVT if you:
- Drink alcohol heavily
- Smoke heavily or use illegal drugs, such as amphetamines and cocaine
- Have coronary artery disease, have had heart surgery or other heart problems
- Have congenital heart disease
- Take over-the-counter cough and cold medicines or prescription medications that can cause a SVT episode
- Have obstructive sleep apnea
Although it is less common, atrial or SVT is sometimes associated with heart attack.
Symptoms and complications
Some people with atrial or supraventricular tachycardia may have no symptoms. Others may experience:
- Fainting (syncope)
- Lightheadedness or dizziness
- Rapid heartbeat or palpitations
- Fluttering in the chest
- Bounding pulse
- Chest discomfort
- Shortness of breath
- Fatigue
In extreme cases, people with atrial or SVT may also experience:
- Unconsciousness
- Cardiac arrest
Treatment for Atrial or SVT
If you have atrial or SVT that occurs once in a while, you may not need treatment if you don’t have symptoms or other heart problems.
Episodes of atrial or SVT often can be stopped by one of a few techniques. These actions should be supervised or conducted by a health care professional. They include:
- Carotid sinus massage: A healthcare professional can apply gentle pressure on the neck, where the carotid artery splits into two branches.
- Valsalva maneuver: This consists of holding your nostrils closed while blowing air through your nose.
- Using the dive reflex: This is the body’s response to plunging your face in ice-cold water.
These techniques are most effective when used right after the arrhythmia starts.
Emergency treatment for prolonged periods of certain atrial or SVT may include:
- Cardioversion: A procedure in which a shock is delivered to your heart through paddles or patches on your chest, restoring your heart to a normal rhythm.
- Medications to control your heart rate or restore a normal heart rhythm.
- Surgery to change the pathways in the heart that send electrical signals (this may be recommended in some cases for people who need other heart surgery)
When episodes of atrial or SVT become frequent, treatment may include:
- Catheter ablation: A procedure in which a doctor threads one or more catheters through your blood vessels to your heart to deliver heat, extreme cold or radio frequency energy to scar a small spot of heart tissue. This blocks the pathway causing your arrhythmia.
- Daily medications to prevent episodes.
- Pacemaker to override the fast heartbeat.
- Surgery to correct the electrical signals causing the abnormal heart rhythm.
In patients with symptomatic Wolff-Parkinson-White Syndrome, medications or ablation may be needed to control paroxysmal supraventricular tachycardia (PSVT).
Preventing Atrial or SVT
Preventing atrial or SVT can be more difficult than treatment. But making the following lifestyle changes may help:
- Cutting down on caffeinated beverages
- Cutting down on alcohol
- Quitting tobacco use
- Eating heart-healthy foods, exercising and maintaining a healthy weight
- Keeping blood pressure and cholesterol levels under control
- Maintaining follow-up care by taking your medications as prescribed and having regular follow-up appointments with your health care professional.
Sinus Tachycardia
Sinus tachycardia is an increase in the heart rate. In this condition, the heart’s natural pacemaker, the sinus node, sends out electrical signals faster than usual.
The heart rate is faster than normal, but the heart beats properly. It’s a common response to exercise, but it’s concerning when it occurs at rest.
Causes of sinus tachycardia
A rapid heartbeat may be your body’s response to common conditions such as:
- Anxiety
- Fright
- Severe emotional distress
- Strenuous exercise
- Fever
- Some medicines and illegal drugs
- Pain
Other, less common causes may include:
- Anemia
- Infection
- Increased thyroid activity
- Heart muscle damage from heart attack or heart failure
- Severe bleeding
- Very low blood pressure
- Lung disease
Treatment
Your doctor should consider and treat the cause of your sinus tachycardia, rather than just treating the condition. Simply slowing the heart rate could cause more harm if your rapid heartbeat is a symptom of a more serious or long-term problem.
Ventricular Tachycardia
Ventricular tachycardia (VT) is a fast heart rate that starts in the heart’s lower chambers (ventricles). Electrical signals in the heart’s lower chambers fire abnormally fast. This interferes with electrical impulses coming from the sinus node, the heart’s natural pacemaker.
The disruption results in a faster than normal heart rate. This rapid heartbeat keeps the heart’s chambers from filling completely between contractions, which compromises blood flow to the rest of the body.
VT may be either well-tolerated or life-threatening, requiring immediate diagnosis and treatment. The severity of VT depends largely on whether you have other heart conditions and the type of VT you have.
Causes of ventricular tachycardia
Ventricular tachycardia is most often associated with disorders that interfere with the heart’s electrical conduction system. These disorders can include:
- Lack of coronary artery blood flow, depriving oxygen to heart tissue
- Cardiomyopathy distorting the heart’s structure
- Medication side effects
- Use of illegal drugs such as cocaine or methamphetamine
- Sarcoidosis (an inflammatory disease affecting skin or body tissues)
- Abnormalities of the heart that result in scarring of heart tissue (sometimes called "structural heart disease"); the most common cause is a prior heart attack
- Congenital heart conditions, including long QT syndrome
- Imbalance of electrolytes necessary for conducting electrical impulses
Symptoms
Symptoms for VT vary. Common symptoms include:
- Dizziness
- Palpitations
- Shortness of breath
- Nausea
- Lightheadedness
- Fainting (syncope)
- Cardiac arrest, in extreme cases
- Chest pain
Treatment
Treatment will depend on your symptoms and the cause of your VT. Possible treatments include:
- Medication that helps prevent arrhythmias
- Radiofrequency ablation, a procedure that destroys the cells causing the VT.
- Surgery to implant a cardioverter defibrillator (ICD), which delivers an electrical pulse to the heart to reset a dangerously irregular heartbeat.
- Immediate electrical defibrillation, in extreme cases