Pub Date: Monday, July 12, 2010
Author: Barry A. Franklin, PhD, FAHA
Article Text
The escalating number of initial and repeat revascularizations in recent years has taught us a sobering lesson: the vessels used to bypass severely stenotic coronary arteries may occlude; evidence of symptomatic or asymptomatic myocardial ischemia may reappear; unbypassed arteries that were previously patent can experience abrupt plaque rupture and occlusion; scar tissue may form at an implanted stent; and other complications (e.g., AMI, stroke) can occur.[2] Accordingly, the IMPACT investigators concluded that future strategies should actively promote population-based prevention by reducing risk factors by lifestyle modification, pharmacotherapies, or both.[1]
Recent studies have reported that four conventional risk factors (cigarette smoking, dyslipidemia, hypertension, diabetes) and obesity, alone or more often in combination, are antecedents in more than 80% of persons who develop CHD.[3-5] Framingham Heart Study participants who were free of cardiovascular risk factors at age 50 were at a very low risk (less than 5% and less than 8% for men and women, respectively) of ever developing the disease.[6] These conventional risk factors and their clinical sequelae are largely preventable with a healthy lifestyle.[7]
As cardiovascular health care providers, we need to become champions of achieving healthy lifestyle overhauls in our patients to facilitate primordial and primary prevention.[8] Our younger patients should be counseled to modify their lifestyles so that they don't gain weight, become habitually sedentary, develop hypertension, hypercholesterolemia, prediabetes or diabetes, or start smoking. For older patients, aged 40 to 50 years, who already have two or more major cardiovascular risk factors, the heightened lifetime risks of developing cardiovascular disease (CVD) (69% for men and 50% for women) suggest the need to become even more aggressive with preventive therapies.[6] The importance of interventions to promote structured exercise, increased lifestyle physical activity and healthy diets in all American adults, is apparent.
Cardioprotective Dietary Recommendations
The American Heart Association's (AHA) 2006 Diet and Lifestyle Recommendations for Cardiovascular Disease Risk Reduction suggest balancing energy intake and energy expenditure to achieve or maintain a healthy weight and choosing a diet that is rich in fish, vegetables and fruits, whole-grain, high-fiber food, and foods with reduced amounts of saturated fat, cholesterol, and salt.[9] These recommendations were echoed in a recent systematic review that found strong evidence of a causal relationship for cardioprotective dietary practices, including vegetables, nuts, and "Mediterranean" eating patterns, and adverse effects of trans-fatty acids and foods with a high glycemic index or load.[10] Another contemporary analysis concluded that modest reductions in dietary salt could substantially decrease future cardiovascular events and associated medical costs.[11] Epidemiologic and controlled interventional studies have consistently demonstrated the cardioprotective effects of omega-3 fatty acid consumption, either from marine sources or via supplements.[12] Fish oils are reported to lessen inflammation, reduce ventricular arrhythmias, decrease triglycerides and lipoprotein levels, and slow the progression of atherosclerosis.[13] In a large meta-analysis including more than 19,000 individuals with documented CVD, omega-3 fatty acid supplementation reduced all-cause and cardiovascular mortality, sudden cardiac death, and stroke.[14]
Physical Activity, Fitness, and Mortality
Numerous epidemiologic studies in people with and without documented CHD have identified low levels of physical activity and cardiorespiratory fitness (aerobic capacity) as independent risk factors for all-cause and cardiovascular mortality (Figure 1).[15] A recent systematic review and meta-analysis of 33 physical activity studies (n = 883,372 participants) reported pooled risk reductions of 35% and 33% for cardiovascular and all-cause mortality, respectively.[16] Similarly, in healthy men and women, each 1 metabolic equivalent (MET; 1 MET = 3.5 mL O2/kg/min) increase in exercise capacity confers a 13% to 15% reduction in mortality.[17] An aerobic capacity ≥7.9 METs identifies a cohort with an excellent long-term prognosis, irrespective of other risk factors or comorbid conditions.[17] Collectively, these data suggest that habitually sedentary patients should be counseled to become more physically active and/or fit by starting an exercise program, increasing lifestyle activity, or both, so as to move them out of the least fit, least active, "high-risk" cohort (bottom 20%).[18]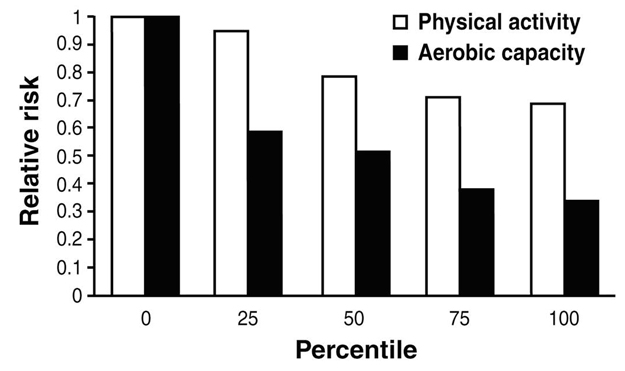
Figure 1. The risks of coronary heart disease and cardiovascular disease decrease linearly in association with increasing percentiles of physical activity. In contrast, there is a precipitous decrease in risk when comparing the lowest to the next-lowest category for aerobic capacity. Beyond this demarcation, the reductions in risk parallel those observed with increasing physical activity but are essentially twice as great for aerobic capacity (cardiorespiratory fitness). Data from Williams.[15]
Counseling Patients Regarding Lifestyle Modification: Contemporary Challenges
According to a telephone survey of 153,000 men and women in the United States, only 3% adhere to four healthy lifestyle characteristics, including not smoking, maintaining a normal body weight, eating adequate daily servings of fruits and vegetables, and exercising regularly. Almost 10% of the respondents adhered to none of these practices.[19] Although physicians and allied health professionals have regular opportunities to counsel patients regarding their lifestyle patterns, many have little or no training in the specific skill sets required for health promotion, especially application of behavioral theory and practice. Unfortunately, most physician practices are also overstretched, and reimbursement for patient counseling and education is suboptimal, to say the least. Despite the well-established benefits of regular physical activity and dietary modifications for cardiovascular risk reduction, less than half of all patients report being counseled about one or both of these lifestyle practices during their most recent physician office visit.[8] Consequently, these and other recent reports suggest that diet and physical activity counseling during ambulatory care visits are often missed, despite data to suggest that brief physician urging during an office visit can favorably modify patient outcomes.
Today, many in the medical community embrace a common treatment approach in the battle against modern chronic diseases: the extrapolation of contemporary pharmacotherapies as a first-line strategy in the prevention of acute cardiovascular events, whether the objective is primordial (prevention of risk factors), primary (treatment of risk factors), or secondary prevention (prevention of recurrent events). As a result, the salutary effects of concomitant lifestyle modification are often overlooked and underemphasized.[20] Lifestyle changes (e.g., smoking cessation, increased physical activity, moderate alcohol consumption) are associated with impressive mortality reductions (20% to 45%), the magnitude of which are similar to or greater than that observed with low-dose aspirin, beta-blockers, statins, and angiotensin-converting enzyme inhibitors (Table 1).[21] Moreover, the effects of lifestyle change and drug therapy on cardiovascular risk reduction appear to be independent and additive.[22-24]
| Intervention | Mortality Risk Reduction |
|---|---|
| Low - dose aspirin | 18% |
| Moderate alcohol | 20% |
| Statins | 21% |
| ß - Blockers | 23% |
| Physical activity | 25% |
| ACE inhibitors | 26% |
| Smoking | 35% |
| Combined dietary changes | 45% |
Table 1. Approximate Morality Reduction Potential of Lifestyle Changes Estimated from Studies in Coronary Artery Disease Patients: Comparison with Preventive Drug Interventions after Myocardial Infarction[21]
Facilitating Behavior Change
The likelihood that patients will or will not engage in a particular lifestyle behavior is governed by a myriad of socioeconomic, attitudinal, and cultural factors, including their expectations of the effects, costs, and consequences of that behavior in relation to their goals and objectives.[8] Behavioral studies have shown that lifestyle change is often characterized by abrupt modulations rather than by gradual movement across a continuum. Accordingly, progressive, regressive, spiraling, or static changes may occur. Unfortunately, too many people believe that lifestyle change is an "all-or-none" phenomenon. Nothing could be further from the truth. Achieving health behaviors that facilitate cardiovascular risk reduction is similar to running a marathon, not a sprint. Thus, patients should be counseled not to become preoccupied about one particular point in the race when they might not have performed as well as they had hoped, and go back to their old ways. The ultimate secret of success is, in a word: persistence. Although most people believe that a single behavior change is easier to make and sustain, multiple simultaneous changes may be easier because they quickly yield perceptible benefits.[25]
The scientific statement by Artinian et al. [26], published in the current issue of Circulation, provides comprehensive evidence-based recommendations on implementing physical activity and dietary interventions among men and women, including adults of racial/ethnic minority and/or socioeconomically disadvantaged populations. To identify investigations pertaining to diet and physical activity behavior change interventions in adults, literature searches were conducted in five databases: MEDLINE, CINAHL, Cardiosource Clinical Trials, Cochrane Library, and PsycINFO. Studies were restricted to those conducted in the United States and published between January 1997 and May 2007. Recommendations for counseling individuals to promote dietary and physical activity lifestyle changes to reduce cardiovascular risk were categorized as Class I, strongly recommended, followed by Class IIa and IIb, where the evidence was generally supportive and less well established, respectively. In contrast, interventions labeled Class III were considered either not useful and/or potentially harmful. Levels of evidence were classified into three tiers: A, sufficient evidence from multiple randomized trials; B, limited evidence from a single randomized trial or other nonrandomized studies; and C, based on expert opinion, case studies, or standard of care.
Cognitive-Behavioral Strategies for Promoting Behavior Change
Artinian et al. [26] summarized the advantages and limitations of commonly employed cognitive-behavior strategies to facilitate behavior change, with specific reference to goal setting, self-monitoring, scheduled follow-up patient contact sessions, feedback and reinforcement, self-efficacy enhancement, incentives, modeling (e.g., having the patient observe another individual engaged in behaviors that are compatible with his/her goals), problem solving and relapse prevention. The role of motivational interviewing, a powerful tool for helping patients to encourage a behavioral transformation, was extensively detailed.[8] To accomplish this, the clinician must convey understanding, acceptance, and interest in the patient as an individual. The first step is to identify the patient's readiness toward changing their behavior by using empathy to identify suboptimal dietary and/or physical activity practices. Getting patients to consciously recognize the circumstances or scenarios that contribute to these behaviors is critical. The next step is getting the individual to understand and accept the need for change. This may entail changing longstanding deleterious behaviors that may be linked to stressful situations, psychosocial variables, work and/or home environments, inadequate education, economic factors, or combinations thereof. Confrontations and arguments must be avoided at this time and interviewers should strive to encourage the patient to hear themselves express why they want to (or should) change. This is most effective using specific questions directed at the patient about why they need to change this behavior. More important, the patient needs to be allowed to speak. The next step is to help the patient overcome inertia and become independent and self-motivating. It is important to emphasize that time is an ally to successful lifestyle modification. Ordinary effort, on a day-to-day basis, can ultimately yield extraordinary results. Finally, patients should be counseled on handling resistance and dealing with recidivism.
Artinian and associates [26] also review the literature regarding the merits of targeting single versus multiple behaviors simultaneously, highlighting print-or media-only delivery strategies, group, individual, technology and multicomponent-based delivery strategies, group-based interventions, individual-focused interventions, and computer/technology-based interventions. The authors emphasized that interventions designed to favorably modify the dietary habits or physical activity practices in one population group may be less effective in another cohort, especially when the population is underserved or economically disadvantaged or differs in cultural health beliefs or practices from the population in which the intervention was initially tested. These interventions should consider the setting in which healthcare is delivered, who delivers the message, cultural sensitivity, literacy level, common barriers to behavior change, and acculturation. The role of additional modulators in initiating and maintaining behavior change is also discussed, including age, gender, health status, co-morbid conditions, cognitive processing, and varied psychosocial factors.
Conclusions
Effective interventions to promote regular physical activity and dietary changes as a population-based preventive strategy will rely heavily on methods, motivation, physician training, and reimbursement practices. Healthcare delivery systems will also need to address a myriad of policy issues to foster an environment that supports the most effective preventive interventions. Patients will need to be directed to individually tailored interventions to circumvent or attenuate barriers to participation and adherence. Recently, the AHA published it's 2020 impact goals, which define cardiovascular health and incorporate seven simple health factors and behaviors, including a healthy diet and adequate physical activity (≥150 minutes/week of moderate intensity or ≥75 minutes/week of vigorous activities, or combinations thereof).[27] Achieving these goals will, no doubt, involve embracing the research-based interventions outlined by Artinian et al. [26], especially those categorized as Class I and IIa, respectively.
References
- Ford ES, Ajani UA, Croft JB, et al. Explaining the decrease in U.S. deaths from coronary disease, 1980-2000. N Engl J Med 2007;356:2388-2398.
- Franklin BA. Coronary revascularization and medical management of coronary artery disease: changing paradigms and perceptions. Eur J Cardiovasc Prev Rehabil 2006;13:669-673.
- Yusuf S, Hawken S, Ôunpuu S, et al. on behalf of the INTERHEART Study Investigators. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet 2004;364:937-952.
- Khot UN, Khot MB, Bajzer CT, et al. Prevalence of conventional risk factors in patients with coronary heart disease. JAMA 2003;290:898-904.
- Greenland P, Knoll MD, Stamler J, et al. Major risk factors as antecedents of fatal and nonfatal coronary heart disease events. JAMA 2003;290:891-897.
- Lloyd-Jones DM, Leip EP, Larson MG, et al. Prediction of lifetime risk for cardiovascular disease by risk factor burden at 50 years of age. Circulation 2006;113:791-798.
- Pearson TA, Blair SN, Daniels SR, et al. AHA guidelines for primary prevention of cardiovascular disease and stroke: 2002 update: consensus panel guide to comprehensive risk reduction for adult patients without coronary or other atherosclerotic vascular diseases. Circulation 2002;106:388-391.
- Franklin BA, Vanhecke TE. Counseling patients to make cardioprotective lifestyle changes: strategies for success. Prev Cardiol 2008;11:50-55.
- Lichtenstein AH, Appel LJ, Brands M, et al. Summary of American Heart Association diet and lifestyle recommendations revision 2006. Arterioscler Thromb Vasc Biol 2006;26:2186-2191.
- Mente A, de Koning L, Shannon HS, Anand SS. A systematic review of the evidence supporting a causal link between dietary factors and coronary heart disease. Arch Intern Med 2009;169:659-669.
- Bibbins-Domingo K, Chertow GM, Coxson PG, et al. Projected effect of dietary salt reductions on future cardiovascular disease. N Engl J Med 2010;362:590-599.
- Psota TL, Gebauer SK, Kris-Etherton P. Dietary omega-3 fatty acid intake and cardiovascular risk. Am J Cardiol 2006;98[suppl]:3i-18i.
- Kris-Etherton PM, Harris WS, Appel LJ, AHA Nutrition Committee. Omega-3 fatty acids and cardiovascular disease: new recommendations from the American Heart Association. Arterioscler Thromb Vasc Biol 2003;23:151-152.
- Wang C, Harris HS, Chung M, et al. n-3 Fatty acids from fish or fish-oil supplements, but not α-linolenic acid, benefit cardiovascular disease outcomes in primary- and secondary-prevention studies: a systematic review. Am J Clin Nutr 2006;84:5-17.
- Williams PT. Physical fitness and activity as separate heart disease risk factors: a meta-analysis. Med Sci Sports Exerc 2001;33:754-761.
- Nocon M, Hiemann T, Müller-Riemenschneider F, et al. Association of physical activity with all-cause and cardiovascular mortality: a systematic review and meta-analysis. Eur J Cardiovasc Prev Rehabil 2008;15:239-246.
- Kodama S, Saito K, Tanaka S, et al. Cardiorespiratory fitness as a quantitative predictor of all-cause mortality and cardiovascular events in healthy men and women. JAMA 2009;301:2024-2035.
- Franklin BA, McCullough PA. Cardiorespiratory fitness: An independent and additive marker of risk stratification and health outcomes. Mayo Clin Proc 2009;84(9)776-779.
- Reeves MJ, Rafferty AP. Healthy lifestyle characteristics among adults in the United State, 2000. Arch Intern Med 2005;165:854-857.
- Franklin BA, Kahn JK, Gordon NF, Bonow RF. A cardioprotective "polypill"? Independent and additive benefits of lifestyle modification. Am J Cardiol 2004;94:162-166.
- Iestra JA, Kromhout D, van der Schouw YT, et al. Effect size estimates of lifestyle and dietary changes on all-cause mortality in coronary artery disease patients: A systematic review. Circulation 2005;112:924-934.
- Sdringola S, Nakagawa K, Nakagawa Y, et al. Combined intense lifestyle and pharmacologic lipid treatment further reduce coronary events and myocardial perfusion abnormalities compared with usual-care cholesterol-lowering drugs in coronary artery disease. J Am Coll Cardiol 2003;41:263-272.
- Chan SY, Mancini J, Burns S, et al. Dietary measures and exercise training contribute to improvement of endothelial function and atherosclerosis even in patients given intensive pharmacologic therapy. J Cardiopulm Rehabil 2006;26:288-293.
- Daubenmier J, Weidner G, Sumner M, et al. The contribution of changes in diet, exercise, and stress management to changes in coronary risk in women and men in the Multisite Cardiac Lifestyle Intervention Program. Ann Behav Med 2007;33:57-68.
- Hyman DJ, Pavlik VN, Taylor WC, et al. Simultaneous vs. sequential counseling for multiple behavior change. Arch Intern Med 2007;167:1152-1158.
- Artinian NT, Fletcher GJ, Mozaffarian D, et al. on behalf of the American Heart Association Prevention Committee of the Council on Cardiovascular and Stroke Nursing. Interventions to promote physical activity and dietary lifestyle changes for cardiovascular risk factor reduction in adults: a scientific statement from the American Heart Association. Circulation 2010. Published online before print July 12, 2010. 10.1161/CIR.0b013e3181e8edf1.
- Lloyd-Jones DM, Hong Y, Labarthe D, et al. on behalf of the American Heart Association Strategic Planning Task Force and Statistics Committee. Defining and setting national goals for cardiovascular health promotion and disease reduction. The American Heart Association's strategic impact goal through 2020 and beyond. Circulation 2010;121:586-613.